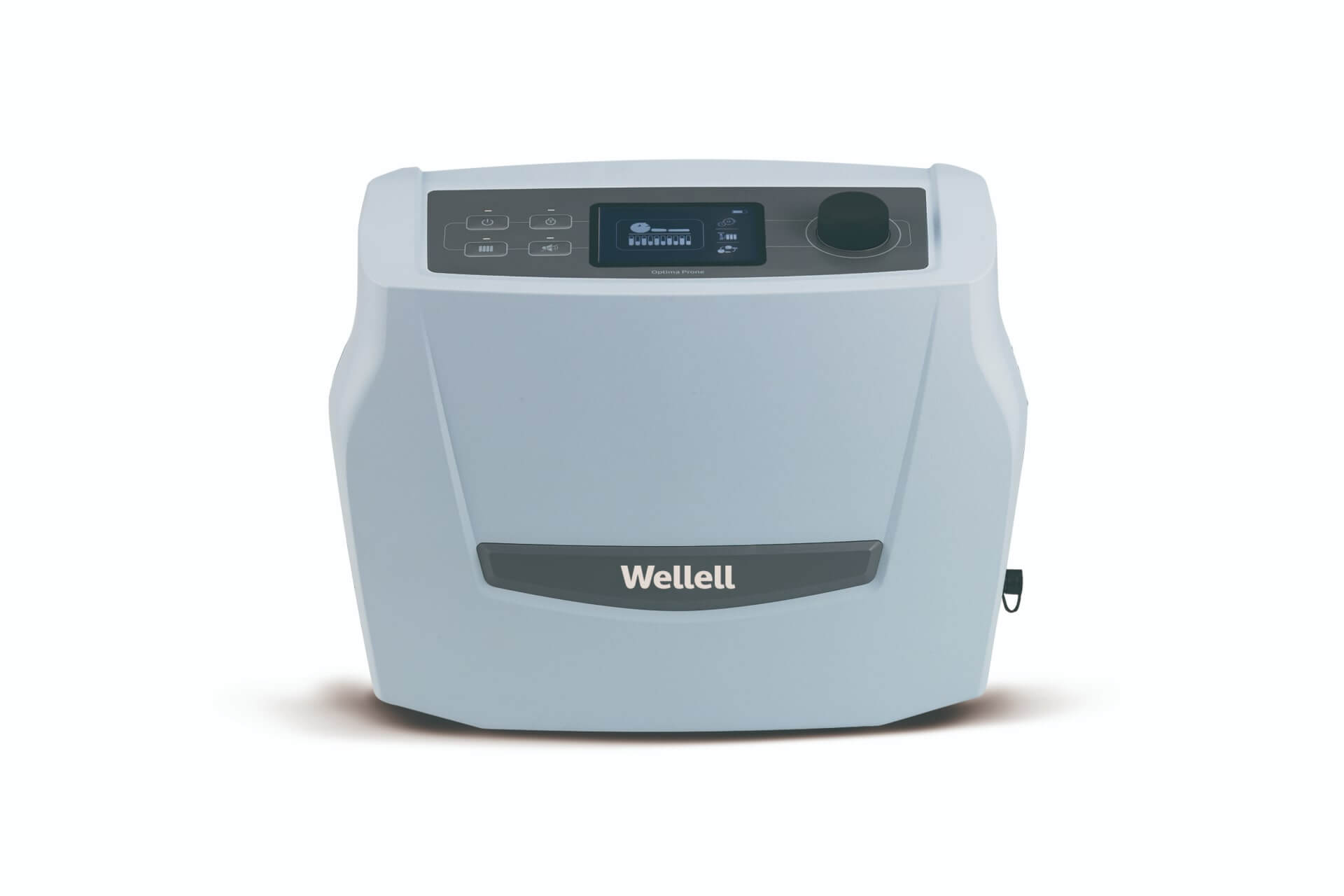
Optima Prone
For High to Very High Risk
Prone Position Pressure Injury Solution — Automating and optimizing prone shoulder lifting and full-body pressure relief
Abbreviations: ARDS, acute respiratory distress syndrome; PPV, prone positioning ventilation.
ARDS accounts for 10% of ICU admissions and 40% of hospital mortality and often requires mechanical ventilation and over 4 weeks of hospitalization. PPV quickly and significantly improves ARDS patients' mortality rate, associated complications risk, and invasive intubation prevention.1-4
Traditional head repositioning and pressure injury prevention during prone positioning are highly complex and labor-intensive. They increase the risk of injuring caregivers and patients significantly, diminishing care quality and crippling the already-insufficient healthcare resources and efficiency.
Optima Prone optimizes caregivers' workflow and care quality. Its mechanical shoulder lifting supports single-caregiver head turning, and customizable individual air cell firmness combined with proprietary pressure relieving headrest ensures full-body pressure injury prevention.

Simplify Head Repositioning
Mechanically supporting shoulder lifts while creating space below the patient's chin decreases the caregiver's workload and risk of obstructing airway tubing, allowing the single-caregiver to perform head repositioning safely and efficiently.

Manage Airway & Fluid Tubing
Deflating individual air cells to guide proper airway and fluid tubing organization prevents potential obstructions or displacements to hemodialysis flow and catheters, reducing the burden on the caregiver's workflow.

Control Individual Air Cell Firmness
Knobs along the mattress (one side) enable caregivers to manually inflate/deflate designated cells to improve region-specific pressure relief and pressure injury prevention in vulnerable areas. The supplied cell airflow tracking tool ensures care quality and consistency.

Protect Vulnerable Facial Structures
The proprietary headrest design layers a soft facial pillow with a sculpted ear pocket over the air cells (firmness also individually customizable) that minimizes pressure against patients’ facial and ear tissues during prone positioning and pressure injury risks.
| Standard 200 | ||
|---|---|---|
| Mattress Dimension | 78.7 x 35.4 x 8 in | 2000 x 900 x 200 mm |
| Mattress Weight | 30.8 lb | 14 kg |
| Maximum Patient Weight | 550 lb | 250 kg |
| Narrow 200 | ||
|---|---|---|
| Mattress Dimension | 78.7 x 33.5 x 8 in | 2000 x 850 x 200 mm |
| Mattress Weight | 30.8 lb | 14 kg |
| Maximum Patient Weight | 550 lb | 250 kg |
| Narrow 200 | ||
|---|---|---|
| Mattress Dimension | 78.7 x 31.5 x 8 in | 2000 x 800 x 200 mm |
| Mattress Weight | 30.8 lb | 14 kg |
| Maximum Patient Weight | 550 lb | 250 kg |

Simplify Head Repositioning
Mechanically supporting shoulder lifts while creating space below the patient's chin decreases the caregiver's workload and risk of obstructing airway tubing, allowing the single-caregiver to perform head repositioning safely and efficiently.

Manage Airway & Fluid Tubing
Deflating individual air cells to guide proper airway and fluid tubing organization prevents potential obstructions or displacements to hemodialysis flow and catheters, reducing the burden on the caregiver's workflow.

Control Individual Air Cell Firmness
Knobs along the mattress (one side) enable caregivers to manually inflate/deflate designated cells to improve region-specific pressure relief and pressure injury prevention in vulnerable areas. The supplied cell airflow tracking tool ensures care quality and consistency.

Protect Vulnerable Facial Structures
The proprietary headrest design layers a soft facial pillow with a sculpted ear pocket over the air cells (firmness also individually customizable) that minimizes pressure against patients’ facial and ear tissues during prone positioning and pressure injury risks.
Reducing prone procedure complexity and caregivers’ workload, and improving patient care and outcome.

Proning reduces intubation and mortality rate for ARDS.
Early prolonged prone-positioning treatment for respiratory-distressed patients improves blood oxygenation (PaO2/FiO2 ratio), prevents further complications, and reduces mortality rate, acute care admissions, and in-hospital days.5,6
No. During this time, the Automatic Pressure Adjustment is inactive and will not be detecting the patient's weight.
Deflation should follow the location of the patient's vulnerable areas. Our recommendations are:
- Head section (supine): 1 cell between cell No. 1 to No. 3
- Head section (prone): All cells between cell No. 1 to No. 3
- Torso section: 2 cells between cell No. 5 to No. 15
- Lower leg section: 1 cell between cell No. 16 to No. 21
The Shoulder Lifting Mode activates a mechanical apparatus that lifts and holds the patient's shoulders and chest upward, mimicking traditional prone positioning therapy's manual shoulder lifting procedure done by two or more caregivers. The lift helps release neck pressure that often leads to hyperextension injury and avoid spinal deformity body pains.
Caregivers have 10 minutes to reposition the patient's head while the mechanical apparatus assists in lifting the shoulders and chest upward. After 10 minutes, the mode automatically deactivates and returns to initial settings. Caregivers can cancel anytime during the procedure through the pump's interface.
In addition to lifting and supporting the patient's shoulder and chest upwards, the Shoulder Lifting Mode also deflates the area below the patient's chin, creating space for the caregiver to secure a steady hold and turn the head while safely managing and preventing airway tubing obstructions.
Yes. Alternating pressure will automatically take over once the Supine Position Mode or Prone Position Mode deactivates after 20 minutes of operation.
Aside from deflating individual cells to relieve pressure on the patient's vulnerable areas, caregivers can do the same but, with less intensity, for other body parts like the abdominal area, which is often protruding and easy to experience discomfort.
Optima Prone's Transport Mode refers to the combination of:
- An optional battery pack that provides non-stop alternating pressure relief for up to 6 hours and,
- The standard 24-hour Wellell mattresses stay inflated (if individual air cells are not adjusted).
All air cells are made from Thermoplastic Polyurethanes (TPU). It is highly resistant to breaking down when in contact with water (hydrolysis), soft to touch, and minimizes friction and noise during patient movements.
Reference
- Force, A. D. T., Ranieri, V. M., Rubenfeld, G. D., Thompson, B., Ferguson, N., Caldwell, E., ... & Slutsky, A. S. (2012). Acute respiratory distress syndrome. Jama, 307(23), 2526-2533.
- Guérin, C., Reignier, J., Richard, J. C., Beuret, P., Gacouin, A., Boulain, T., ... & Ayzac, L. (2013). Prone positioning in severe acute respiratory distress syndrome. New England Journal of Medicine, 368(23), 2159-2168.
- Guerin, C., Beuret, P., Constantin, J. M., Bellani, G., Garcia-Olivares, P., Roca, O., ... & Mercat, A. (2018). A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive care medicine, 44, 22-37.
- Ding, L., Wang, L., Ma, W., & He, H. (2020). Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Critical care, 24, 1-8.
- Coppo, A., Bellani, G., Winterton, D., Di Pierro, M., Soria, A., Faverio, P., ... & Foti, G. (2020). Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. The Lancet Respiratory Medicine, 8(8), 765-774.
- Guérin, C., Reignier, J., Richard, J. C., Beuret, P., Gacouin, A., Boulain, T., ... & Ayzac, L. (2013). Prone positioning in severe acute respiratory distress syndrome. New England Journal of Medicine, 368(23), 2159-2168.